Diabetic retinopathy
What is Diabetic Retinopathy?
Diabetic retinopathy is a secondary disease of diabetes. In those affected, high blood sugar damages the retina and leads to vision loss. Diabetic retinopathy occurs in both type 1 and type 2 diabetes.
Diabetes is a very insidious disease. Your body is unable to produce the hormone insulin. Without sufficient insulin supply, carbohydrates cannot be metabolized for energy production, sugar accumulates in the blood and damages many organs. The fatal consequences are changes in the blood vessels. Diabetes cannot be cured, but it can be controlled by lowering blood sugar levels with insulin and other drugs. Unfortunately, we cannot always control the situation in such a way that we can avoid all related problems.
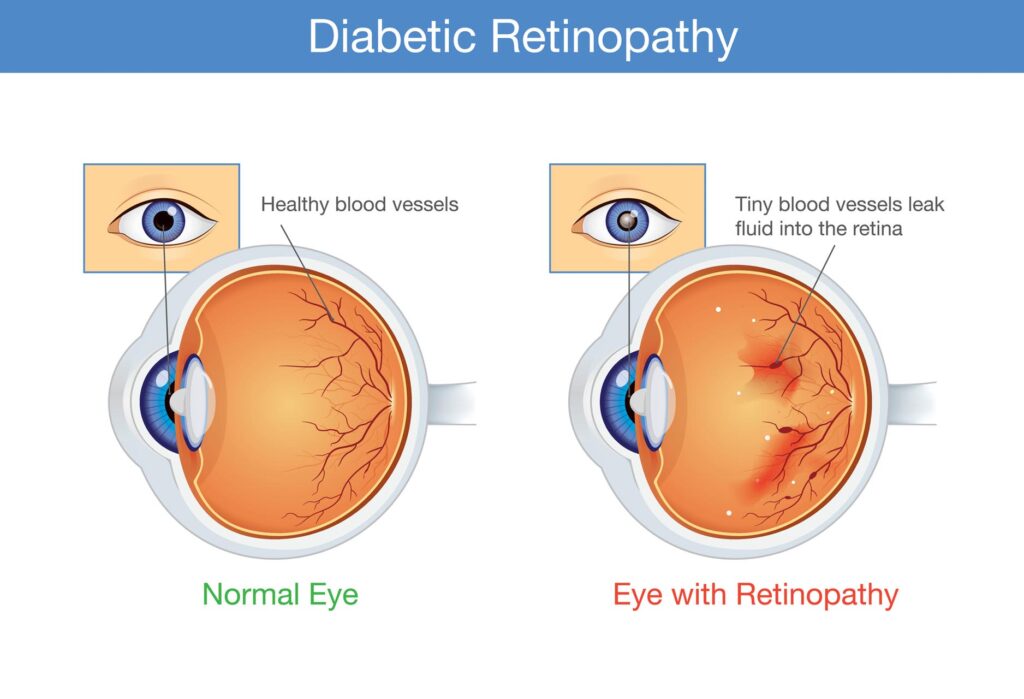
The retina consists of specialized nerve cells (photoreceptors) that convert light rays entering the eye into nerve impulses. Elevated blood sugar levels change the blood vessels that supply nutrients to the retina. The small blood vessels in the retina are damaged, causing the photoreceptors to get too little oxygen.
In advanced stages, new but unstable blood vessels form there. As a result, fluid or blood leaks out of the vessel and leads to new vascular branches. Those affected progressively lose their sight and, in severe cases, can even become completely blind. In Europe, diabetic retinopathy is the leading cause of blindness in adults over 65 years of age, with diabetics being 25 times more likely to go blind than non-diabetics. Duration and end of diabetes are determinants for the development of retinopathy. Only 15% of people with diabetes for 4 years have the disease, but 90% of people with diabetes for 15 years or more have typical vascular changes. Due to modern medical options, only a small percentage of people with diabetic retinopathy experience severe vision loss.
What are the symptoms?
When nerve cells in the retina are damaged, vision gradually deteriorates. It takes years. Especially in the first years of illness, the damage often progresses only slowly. Therefore, those affected do not know about diabetic retinopathy for a long time. However, in later stages, vision deteriorates significantly.
After that, diabetic retinopathy often causes acute symptoms. Warning signs are generally sudden changes in vision. Especially when the macula is diseased, it is almost impossible for the person affected to read: vision is blurred or color perception is different. When a blood vessel in the retina ruptures and the retina bleeds, a black spot suddenly appears in the field of vision. Bleeding often also affects the vitreous of the eye (vitreous hemorrhage). The patient sees black dots running (“soot rain”).
In addition, progressive diabetic retinopathy causes retinal detachment (retinal detachment). This is noticeable, for example, through flashes of light and dark shadows. This is noticeable, for example, through flashes of light and dark shadows.
What causes diabetic retinopathy?
Diabetic retinopathy is caused by persistently high blood sugar levels. The worse your blood sugar is controlled, the more likely you are to develop diabetic retinopathy.
In sufferers, high levels of sugar molecules in the blood damage the lining of the smallest blood vessels (capillaries). This damage is also known as microangiopathy. All small blood vessels in the body are affected, but especially the retinal vessels, kidney vessels and in general the vessels that supply nerve cells in the body.
Nerve cells in the retina die when they are deprived of adequate blood and oxygen due to damaged blood vessels. There is also a risk that damaged capillaries will leak. This applies in particular to blood vessels that the body forms to compensate for deficiency symptoms. Unstable and easy to lick. The resulting blood leakage causes additional damage to the retina.
Diabetic retinopathy treatment: This is how the preservation of vision is favored
While diabetic retinopathy in most cases leads to complete vision loss if left untreated, the disease is now easily treatable. In order to achieve the best possible success in this regard, those affected should consult an ophthalmologist if they suspect diabetic retinopathy or changes in the eye or vision. In addition, a healthy lifestyle is beneficial to minimize the risk of complications like these. It is true that side effects such as diabetic retinopathy cannot be completely prevented in the case of diabetes, but a healthy lifestyle can make a massive contribution to keeping the risk of suffering from subsequent diseases as low as possible. Sufficient exercise should therefore be integrated into everyday life, as should a balanced diet and abstinence from alcohol and smoking. Adjusted insulin administration and regular monitoring of blood sugar and blood pressure are also necessary.
Treatments for proliferative diabetic retinopathy include:
However, if diabetic retinopathy occurs, especially proliferative retinopathy, the retina of the eye does not have sufficient blood supply. This leads to vascular damage, which in turn leads to the formation of new vessels, which, however, develop abnormally. The new vascular proliferations are usually located on the vitreous side and cause problems for the patient due to their inferiority and abnormal shape. Bleeding and leakage of fluid from the eye are just some of the consequences.
To prevent this and to help preserve vision, laser therapy is used, which aims to stop the leakage of fluid from the vessels in the retina, resulting in stabilization of the retina.
In the course of the therapy, all areas of the retina that ensure fluid permeability are first determined using fluorescence angiography. The permeable areas are then sclerosed with a laser and sealed in this way. Scarring of the tissue ultimately ensures that no more liquid can escape from the relevant areas.
Even if this type of therapy is crowned with success and leads to an improvement in vision, repeated treatments can be expected. The leakage of liquids cannot always be prevented by means of laser therapy, especially since further abnormal vascular formation is to be expected in proliferative retinopathy, which in turn promotes the leakage of liquids. Another disadvantage that patients can expect is peripheral vision loss. However, since the therapy aims to preserve central vision, effects such as these should not result in the forgoing of appropriate therapy.
In extreme cases, the formation of new vessels is very pronounced and if there is bleeding in the vitreous body, proliferation of blood vessels or a detachment of the retina due to scarred tissue, a major surgical intervention is usually indispensable. A vitrectomy is usually carried out here, which is intended to promote the preservation of vision. In addition to scar tissue and proliferation of the vessels, the vitreous itself is also removed in this way. More than 60 percent of all patients treated can look forward to an improvement in their vision in this way.
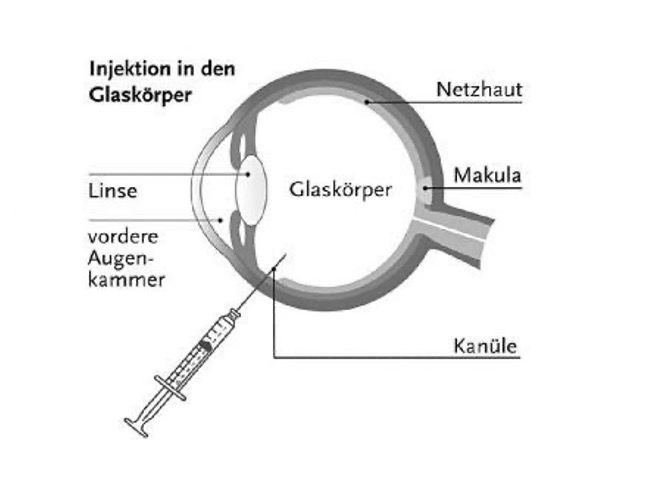
A buildup of vascular fluid, also known as diabetic macular edema, can also be treated with intravitreal injection, or IVOM for short, using drugs called antivascular endothelial growth factor. If the morphological macular findings indicate a high probability of an improvement in vision through IVOM, therapy can be started. The medication is injected directly into the vitreous with a needle under local anesthetic and under sterile conditions.
Drugs approved for this occasion, all of which belong to the group of anti-VEGF preparations, include:
-
Ranibizumab (trade name Lucentis®)
-
Aflibercept (trade name Eylea®)
-
Brolucizumab (Beovu®)
-
Bevacizumab (trade name Avastin®)
The above VEGF inhibitors are contained in the injections. The IVOM treatment is usually painless.
Even if treatment helps to improve the symptoms and vision immediately, the duration of the effect of the medication is limited, so that further treatments are necessary. As a rule, a series of treatments is carried out, which consists of three injections, which are administered four to twelve weeks apart. Further regular checks should be carried out in order to detect the renewed formation of abnormal vessels in good time.