Macular degeneration
What is meant by macular degeneration?
At the very beginning, it should be clarified what is meant by macular degeneration. Overall, this is a destruction of the macula. This in turn is an extremely sensitive area on the back wall of the eye. In general, incoming light is directed to the retina. Thanks to the light-sensitive membrane, images are captured like the film of a camera and converted into images. The entire retina is important for good vision. However, there is one central spot that is about 100 times more sensitive than any other. And that is the aforementioned macula.
It has many cones, which are responsible for detailed vision and the recognition of different colors. Without a functioning macula, it is impossible to see detail. This includes, for example, a colored world and printed letters.
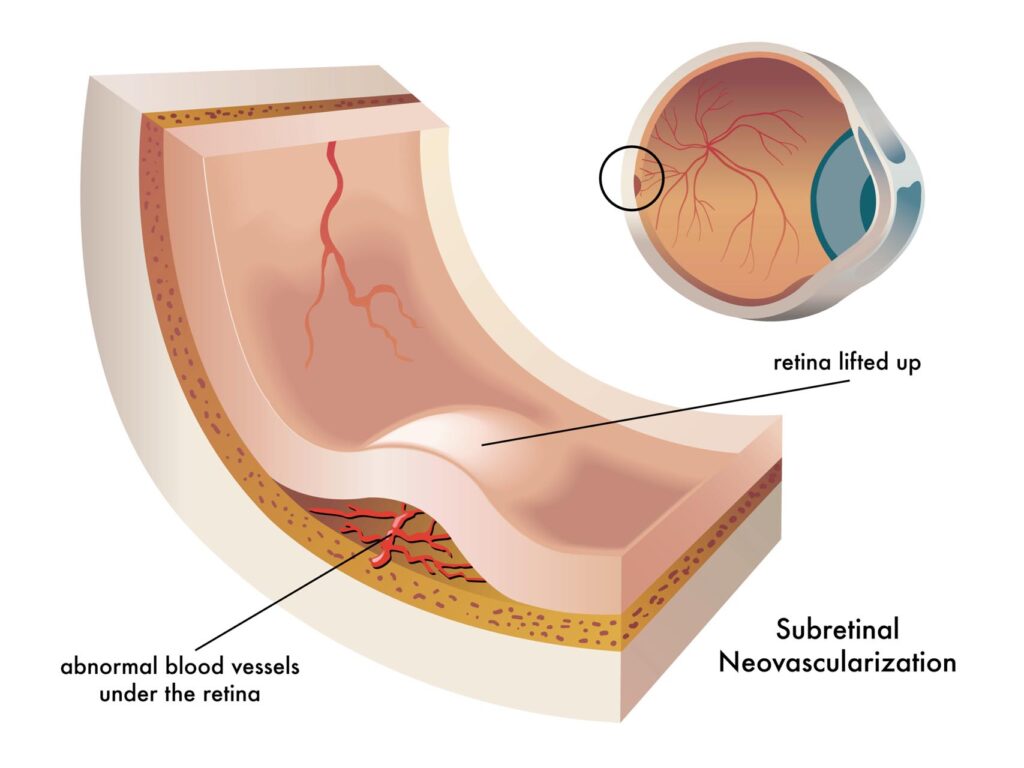
Wet macular degeneration: Wet macular degeneration occurs in 15% of patients, but it has a severe course. This leads to a faster progressive vision loss. New semipermeable blood vessels grow from the choroid beneath the retina. As a result, bleeding, swelling and scars occur. If left untreated, it can cause vision to deteriorate more quickly. This can lead to a severe loss of near and far vision, making everyday activities such as reading and driving impossible.
What are the causes of macular degeneration?
Destruction of the macula sounds anything but good at first glance. But what exactly are the causes? Destruction can happen through a variety of things. Depending on the condition, the disease can also occur in both eyes at the same time. In advanced stages, it is possible to lose central vision. It does not lead to total blindness, however, since peripheral vision is unaffected.
Age is one of the main causes in Europe. Central vision loses strength in over a third of those over the age of 65. However, the disease can develop at any age. Basically, a distinction is made between different types. And these are:
Wet macular degeneration: Wet macular degeneration occurs in 15% of patients, but it has a severe course. This leads to a faster progressive vision loss. New semipermeable blood vessels grow from the choroid beneath the retina. As a result, bleeding, swelling and scars occur. If left untreated, it can cause vision to deteriorate more quickly. This can lead to a severe loss of near and far vision, making everyday activities such as reading and driving impossible.
1) dry form
The most common form of macular degeneration is the dry form. In this case, the sensitive tissue of the macula has degenerated and its function is severely impaired. However, it appears to be part of the general aging process.
2) wet form
The wet form is a little different. It occurs much less frequently, but is correspondingly more dangerous. The growth factor performs essential functions in the formation of new blood vessels throughout the body. For this reason, inhibitors against this growth factor have been developed. The extent and damage depend entirely on the extent and duration of the process.
What symptoms can macular degeneration cause?
At least as important are the symptoms by which those affected can recognize a possible macular degeneration. As already mentioned, the disease can develop in different ways. So the symptoms can vary accordingly. Classic symptoms include:
-
A progressive loss of the ability to recognize objects
-
Distorted vision where objects appear abnormally large
-
Dark or empty space in the visual center
However, patients who suffer from any of the symptoms listed above should not immediately assume that they suffer from this particular disease. Only when objects and colors are clearly recognized in a different color does the doctor have to be consulted. Because it is not uncommon for one of the above-mentioned problems to be compensated for by the other eye. When you get to the doctor, different tests are carried out. An examination with the indirect ophthalmoscope takes place. This is followed by a test with the Amsler network. If everything is then correct, there is still an OCT – coherence tomography of the macula. A color vision test should also not be missing.
How can macular degeneration be treated?
But how exactly can the disease be treated by a specialist? There is no effective treatment for most cases in this area. Because once the destruction of the retina has begun, it is hardly possible to heal it or to regenerate damaged cells. There is currently no known treatment that can be used to stop the dry form.
In the wet form, on the other hand, the complete central vision is destroyed without control. In the end, only peripheral vision remains. By this form, a buildup of vascular fluid, in or under the macula, also known as macular edema, can also be treated with intravitreal injection, or IVOM for short, using drugs called antivascular endothelial growth factor (anti-VEGF). If the morphological macular findings indicate a high probability of an improvement in vision through IVOM, therapy can be started.
The medication is injected directly into the vitreous with a needle under local anesthetic and under sterile conditions.
Drugs approved for this occasion, all of which belong to the group of anti-VEGF preparations, include:
-
Ranibizumab (trade name Lucentis®)
-
Aflibercept (trade name Eylea®)
-
Brolucizumab (Beovu®)
-
Bevacizumab (trade name Avastin®)
The above VEGF inhibitors are contained in the injections. The IVOM treatment is usually painless.
Treatment
Even if treatment helps to improve the symptoms and vision immediately, the duration of the effect of the medication is limited, so that further treatments are necessary. As a rule, a series of treatments is carried out, which consists of three injections, which are administered four to twelve weeks apart. Further regular checks should be carried out in order to detect the renewed formation of abnormal vessels in good time.